Arizona nonprofit aiding COVID-19 protocol victims.
Loss of Faith in the Healthcare System
There was a time when Kurtis Bay of Arizona believed in the health care system and that the Hippocratic Oath to “do no harm” had real meaning.
His ultimate loss of faith followed the complete loss of medical freedom he experienced in January 2022 when his wife, Tammy, went to the emergency room at a Phoenix-area hospital for a respiratory ailment.
“My wife did not have COVID. She did not test positive for COVID”—that’s what the emergency room staff told him when they admitted her on Jan. 5, 2022, Mr. Bay told The Epoch Times.
They told him instead that she had pneumonia but ”isolated her” in the COVID unit anyway. They labeled him “combative” for wanting answers about his wife’s condition.
Then they called the police and issued a no-trespass order against him, which meant he couldn’t see his wife unless the hospital permitted him.
And when Tammy died in the hospital several days later, at age 59, having twice been intubated and placed on a respirator against her husband’s instructions, the official cause of death was “sepsis and COVID-19.”
Related Stories
The Truth About COVID Hospital Protocols: Stella Paul
10/17/2023
Class-Action Lawsuit Filed Against Remdesivir Manufacturer Over Alleged Deceptive Practices
9/30/2023
“If they had treated Tammy for what she was in there for, she’d be alive today,” said Mr. Bay, a member of the board of directors of the nonprofit COVID-19 patient rights advocacy group “1,000 Widows.”
Mr. Bay joined the grass-roots organization in 2022 to help others who said they lost loved ones to standard medical protocols during the government-declared pandemic.
Mr. Bay said he realized there were many others just like him—more than 30,000 in the group—who were just as “confused or had no idea this was occurring” throughout the hospital system.
On its website, the group said its primary mission is to raise awareness of the “destruction of countless lives during the pandemic” with a focus on civic action and community support.
Members can also access financial and mental health resources and information through faith-based initiatives.
As important, Mr. Bay said, are 1,000 Widows’ legislative efforts to strengthen medical freedom and accountability with a revised Arizona patient bill of rights.
The group helped overturn Arizona SB1377, pandemic legislation that declared a medical health provider immune to liability for negative outcomes if it acted in “good faith” during a public health emergency.
“COVID-19 patients in Arizona who feel they were harmed by healthcare providers during the pandemic are now able to pursue legal claims and seek damages,” said 1000 Widows member Sara Behmer-Pinheiro in a letter to The Epoch Times.
“Our vision is to create a world where families impacted by tragedies, like the COVID-19 pandemic, can access real-time support and resources tailored to their unique needs.
“We aim to bring together individuals, organizations, and partners from all walks of life, fostering a community that stands together in times of crisis.”
One Arizona lawmaker who supports the group is Sen. Janae Shamp, a Republican member of the state legislature’s Coronavirus Southwestern Intergovernmental Committee.
On Oct. 20, the body met in Phoenix to hear presentations on COVID-19 protocols, autopsy findings, and ways to protect medical and religious vaccine exemptions.
“While I believe that there is a need to review and enhance the patient’s bill of rights, we will not be discussing a formal proposal at this hearing,” Ms. Shamp, vice-chairwoman of Arizona’s Health and Human Services, told The Epoch Times.
“However, the general concept of the patient’s bill of rights is an important and unavoidable component of the discussion we will be having regarding proper informed consent, adverse events, and other implications of the widespread deployment of COVID-19 vaccines and other related countermeasures.”
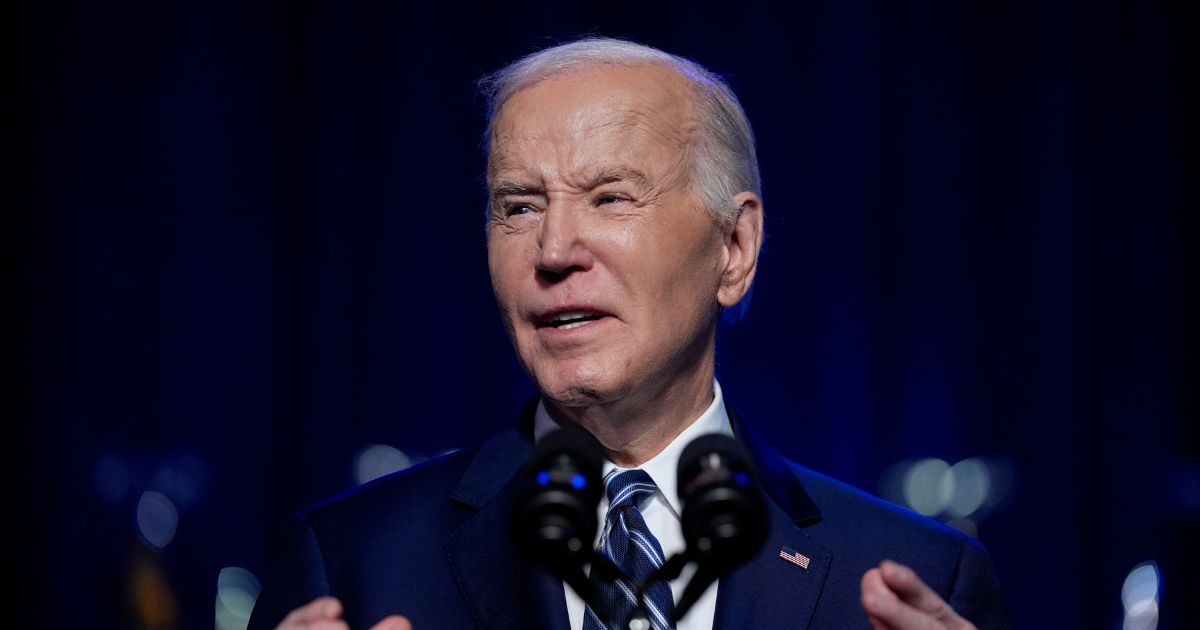
On May 11, the Biden administration ended the COVID-19 pandemic health emergency declaration, allowing government health agency authorizations for collecting medical health data to expire.
In late 2020, the World Health Organization (WHO) issued a conditional recommendation against the use of the antiviral drug Remdesivir in hospitalized COVID-19 patients, “regardless of disease severity, as there is currently no evidence that Remdesivir improves survival and other outcomes in these patients.”
Remdesvir is one of two National Institutes of Health (NIH) preferred therapies after the antiviral Paxlovid used to prevent hospitalization for COVID-19, according to Yale Medicine.
However, at least two studies linked the drug’s use to acute kidney injury in COVID patients.
“Once you arrive, they put you into a particular process,” Mr. Bay said, noting that some hospitals still use peak COVID-19 protocols to treat patients.
“It doesn’t matter what your loved one came in with. They don’t have to be COVID-positive. They can still treat them for COVID whether they are COVID-positive or not. They can move them in this system and check the box for the [government financial] incentive plan,” he said.
The incentive plan Mr. Bay referred to provides hospitals with enhanced payments for COVID-19 diagnoses under the Coronavirus Aid, Relief, and Economic Security (CARES) Act.
‘Had A Feeling’
Although Kurtis and Tammy Bay were unvaccinated for COVID-19, they were not anti-vaccine. They were, however, skeptical about putting an experimental chemical into their bodies, despite both contracting the virus during the pandemic.
“We called it the sleeping disease because we were tired for 10 or 12 days [but] we were fine,” Mr. Bay said.
The night Tammy experienced chest discomfort on Jan. 5, 2022, the couple were on their way to an urgent care facility after hours.
“Are you taking me to the emergency room?” Tammy asked her husband, who said, “No.”
“Well, I think that’s where I’m going to end up,” Tammy said. “I just have a feeling.”
Mr. Bay said his wife’s apprehensions were correct. And when the hospital admitted her hours later, he wrote on a medical whiteboard: “No sedation. No high-flow oxygen. No Remdesivir.”
Within 24 hours of her admittance, “they were already sedating her,” he said. “I was labeled combative on the first day. They called security to try to remove me. The cops came, and I was trespassed.”
On day three, Mr. Bay requested a transfer for Tammy—and on that day, they intubated her. A panic attack landed her in the intensive care unit, simply because of the hospital’s COVID-19 protocol for elevated breathing and heart rate.
One night, Tammy called her husband, pleading to come and take her home—”and I couldn’t—I couldn’t come and get her,” Mr. Bay said, breaking into tears. “They wouldn’t let me.”
“They were following a regimen. Nobody asked how Tammy was feeling. They didn’t even know her [expletive] name.”
Tammy eventually developed a leaking perforation in her bowel that required emergency surgery.
“All of this happened because she was in the hospital,” said Mr. Bay, who received the devastating news that Tammy couldn’t have the life-saving operation.
The surgeons said that to do the procedure, Tammy would have to lie on her stomach. If that happened, she would stop breathing and die. Without the surgery, her body would become septic and she would die.
“So I said goodbye to her,” Mr. Bay said. “And that’s the way it went.”
On Jan. 20, 2022, Tammy took her last breath—two weeks after her hospital admittance for pneumonia, her husband said.
Mr. Bay said the medical bill from the insurance company—more than $300,000—was like adding insult to injury.
With COVID-19 as a post-mortem diagnosis, the hospital received $12,000 under the CARE Act, he said.
“It’s still happening today—the same protocols. It doesn’t matter whether you give consent or not,” he said.
Mr. Bay said a “driving message” from 1,000 Widows members is their shared desire for justice and medical accountability denied by the legal establishment.
“It was clear we needed to establish more local and civic responsibility in the form of legislation,” Mr. Bay said.
“This isn’t about me. It isn’t about my wife. It’s about us—the victims. None of us wants to be here. But here we are.”
Rections and Criminal Justice Committee.
How does the Reactions and Criminal Justice Committee address systemic issues in the criminal justice system?
The Reactions and Criminal Justice Committee addresses systemic issues in the criminal justice system through various measures. Some of these measures may include:
1. Research and Analysis: The committee conducts in-depth research and analysis of the criminal justice system to identify areas of systemic issues. This may involve examining patterns of bias, discrimination, or inequality within the system.
2. Policy Advocacy: Based on their research, the committee may advocate for changes in legislation and policies that address systemic issues. This could involve proposing reforms to laws, procedures, or practices to promote fairness, reduce racial disparities, or enhance rehabilitation.
3. Public Awareness and Education: The committee promotes public awareness and education about systemic issues in the criminal justice system. This could involve organizing seminars, workshops, or public forums to engage with communities, raise awareness, and encourage dialogue on these issues.
4. Collaboration with Stakeholders: The committee collaborates with various stakeholders, including law enforcement agencies, legal professionals, community organizations, and advocacy groups. By working together, they can develop strategies to address systemic issues and implement necessary changes.
5. Monitoring and Evaluation: The committee continuously monitors and evaluates the impact of policies and measures undertaken to address systemic issues. This helps in identifying strengths and weaknesses, making adjustments, and ensuring that systemic changes result in meaningful improvements within the criminal justice system.
By employing these strategies, the Reactions and Criminal Justice Committee aims to tackle the root causes of systemic issues and promote a fair, just, and effective criminal justice system.
" Conservative News Daily does not always share or support the views and opinions expressed here; they are just those of the writer."