Medical Industry Doesn’t Want You To Know About IVF Alternatives
Physicians recently convened in Washington, D.C. to discuss differing approaches to addressing the growing infertility crisis. representatives from the American Society for Reproductive Medicine (ASRM) and the International institute for Restorative Reproductive Medicine (IIRRM) provided contrasting perspectives during congressional briefings. The White House has promoted expanding access to in vitro fertilization (IVF) as a public policy solution, but IVF remains costly, invasive, and ethically controversial, with relatively low success rates.
In contrast, Restorative Reproductive Medicine (RRM) is gaining attention as a holistic approach that focuses on understanding and improving a woman’s reproductive health through cycle tracking and identifying treatable underlying causes of infertility, such as hormonal imbalances and thyroid issues. Advocates argue RRM is less invasive,more affordable,and results in better maternal and neonatal health outcomes. Several organizations and clinics actively support and practice RRM.
The debate is heated, with groups like ASRM criticizing RRM as unproven and ideologically driven, while RRM supporters defend the approach with international data demonstrating positive results. Patient voices and personal stories shared at the congressional meetings emphasized the potential benefits and growing demand for RRM. Advocates hope to increase awareness and integration of RRM into fertility care as part of a comprehensive response to the nation’s fertility challenges.
Physicians gathered in Washington, D.C. last week to present divergent views on treating the rising rate of infertility.
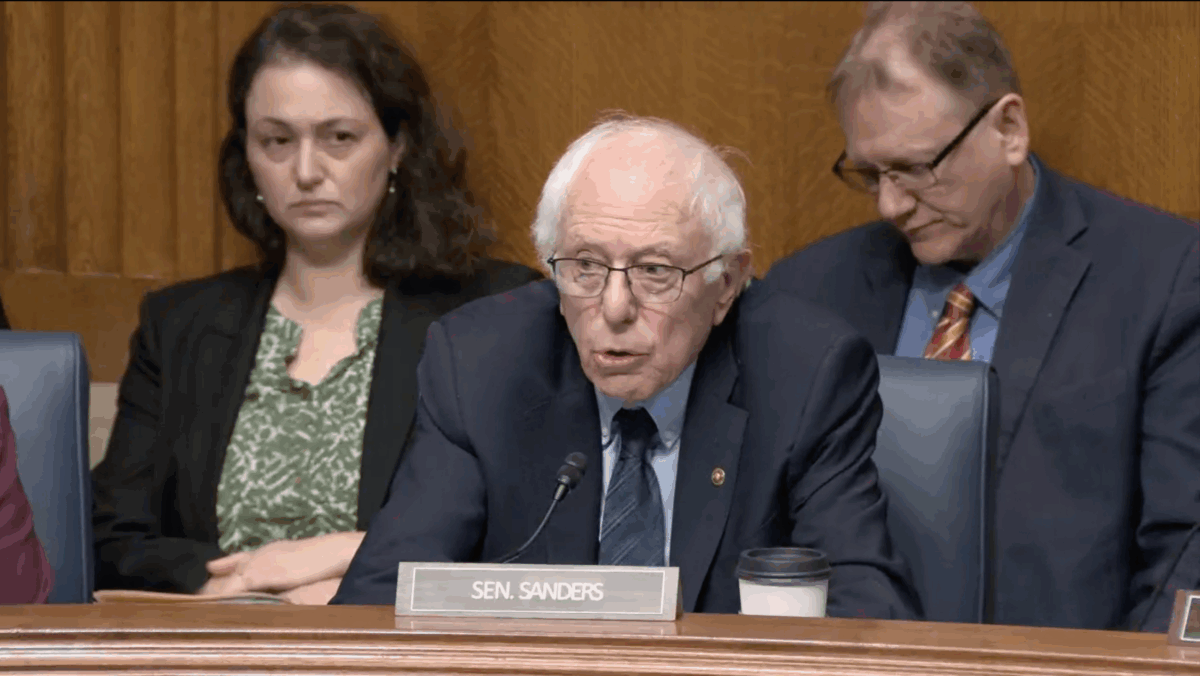
Members of the American Society for Reproductive Medicine (ASRM) and the International Institute for Restorative Reproductive Medicine (IIRRM) held separate congressional briefings before lawmakers, staff, physicians, and patients as part of an increasingly public debate on treating the nation’s declining birth rate.
In February, a White House executive order promised to expand access to in vitro fertilization (IVF) as a solution to population decline; a “public policy” move to “make it easier for loving and longing mothers and fathers to have children.”
But IVF is expensive, costing upwards of tens of thousands of dollars per cycle, and contains ethical and practical failures; rates of successful conception through IVF remain low, and embryos are regularly discarded in the process.
Alternatively, whole-person fertility care, known as Restorative Reproductive Medicine (RRM), is gaining increasing popularity in public discourse.
A dynamic and evolved care model focused on body literacy, cycle tracking, and individualized women’s health markers, RRM practitioners work to restore a woman’s reproductive health to conceive naturally.
Several large groups and clinics have formed over the years to support and expand this version of care, describing it as the superior option for women and couples. RRM practitioners typically identify treatable underlying causes for infertility, such as low estrogen and progesterone, insulin resistance, thyroid disease or dysfunction, and endometriosis, resulting in improved fertility and healthier patients.
Organizations like FACTS About Fertility, FEMM Health, IIRRM and the Institute of Restorative Reproductive Medicine of America, all stand behind this model, while clinics such as NeoFertility, Reply Fertility, and The Gianna Center produce outcomes and supporting data.
Disrupting the Babymaking Market
As the promise of policy to expand access to IVF remains unfulfilled, advocates are feeling the threat of a more successful and financially viable model.
The American College of Obstetricians and Gynecologists (ACOG), a left-leaning and politically charged organization, derided the “so-called” medicine of RRM in a recent publication, claiming it could “expose patients to needless, painful surgical interventions; limit their access to the full range of evidence-based fertility care interventions; and delay time to pregnancy, while potentially increasing overall costs.” It also dismissed the elevation of personhood RRM recognizes in the unborn.
In its response, IIRRM addressed ACOG’s and other medical groups’ “erroneous claims,” including studies from five countries proving significant successes with RRM.
“RRM has a record of care that, compared to IVF, is less invasive, less expensive, and has improved maternal and neonatal health outcomes…” the statement said.
Earlier this month, Dr. Elizabeth Ginsburg, ASRM president, wrote a scathing Op-ed for The Hill calling RRM “dangerous and misleading,” and “an unproven, ideologically driven approach to fertility.” She characterized RRM as a movement intent on the political aim to “get rid of IVF,” warning Americans that a federal funding shift toward RRM, “would have serious consequences for patients.”
Leaders in RRM care disagree.
‘This Is All Hands On Deck’
Political and religious views aside, RRM is “good medicine and good health care,” said Dr. Monica Minjeur, IIRRM U.S. director of communications and development.
“This is all hands on deck,” added Dr. Tracey Parnell. “We are in a fertility crisis; you would think that any physicians with expertise in this field would be a welcome addition.”
RRM physicians were a very welcome addition to Anna Camacho’s life. The nurse practitioner now specializes in RRM after years as a neonatal and family NP. She shared her fertility journey at Tuesday’s meeting on the hill.
Camacho and her husband struggled with infertility early in their marriage and received limited answers from a reproductive endocrinologist who ultimately directed them to IVF, which they refused. They had ethical concerns about IVF, and Camacho’s experience as a neonatal nurse had exposed her to the maternal and fetal risks. After surgery and medication did not result in a child, they explored options outside of traditional care.
They came across RRM but were “skeptical,” until they examined the data, a growing body of international success rates. A thorough workup revealed multiple health issues that had gone undiagnosed for Camacho. Her RRM caregivers addressed each issue, and for the first time in her life, she said she felt physically “better.” She went on to conceive two children and has now helped hundreds of other patients through their fertility journeys.
“Our overarching goal was to get RRM in the conversation at the congressional level, and to bring awareness to the patient voices,” Minjeur said. “We had a lot of patients speaking and honestly, their voices are what drives us and need to be heard. I think it was roaring loud and clear.”
Ashley Bateman is a policy writer for The Heartland Institute and blogger for Ascension Press. Her work has been featured in The Washington Times, The Daily Caller, The New York Post, The American Thinker and numerous other publications. She previously worked as an adjunct scholar for The Lexington Institute and as editor, writer and photographer for The Warner Weekly, a publication for the American military community in Bamberg, Germany. Ashley is a board member at a Catholic homeschool cooperative in Virginia. She homeschools her four incredible children along with her brilliant engineer/scientist husband.
" Conservative News Daily does not always share or support the views and opinions expressed here; they are just those of the writer."